Curriculum Highlights
-
Immersion
Instead of a few days of orientation, our residents begin their training with four weeks of structured learning, designed to aid in transition to residency.
Past Residency classes have rated this extremely helpful in making this transition, and we continure to refine it each year based on residents feed back. Click below to learn more.
-

Outpatient Clinic
Our outpatient curriculum is based on a longitudinal experience in our outpatient clinic on the St. Ann’s Campus. Each resident has their own patient panel for which they serve as the primary care physician. Residents spend a variable number of half-days per week caring for their patients under the supervision of Family Medicine faculty in the FMC, increasing gradually over the course of the residency until the experience mimics an independent practice setting. This the principle learning environment and "home base" throughout the course of residency.
-

Inpatient Medicine
Our primary inpatient service is an unopposed medicine service at St. Ann’s Hospital in Westerville, Ohio. Residents complete 4 four-week blocks of IPS during the PGY-1 year, 4 blocks in PGY-2 and 2 blocks in PGY-3.
-

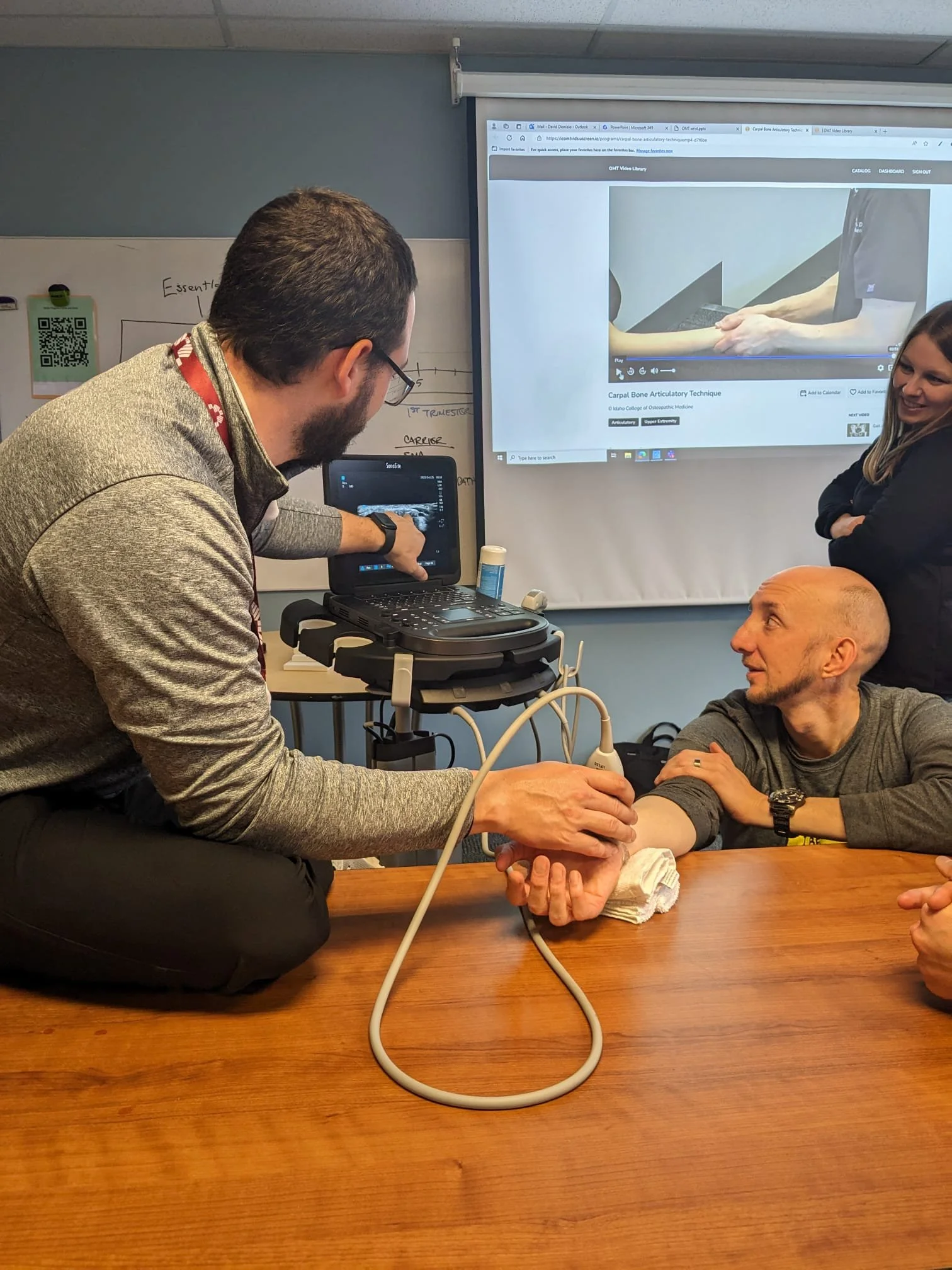
Sports Medicine
Our Sports Medicine Curriculum includes two month-long rotations, regular sessions and procedural workshops as well as sports related volunteer opportunities. PGY-2 residents spend one month in a private orthopedic surgery office and one day a week with Sports Medicine Faculty, Dr. Jonathan Newsom. Residents are involved in a multitude of musculoskeletal evaluations and procedures and receive significant exposure to joint injections. PGY-3 residents spend an additional month dedicated Sports Medicine.
-

Global Health
The Global Health program at Mount Carmel Family Medicine Residency was started by Dr. John O’Handley, program director at SAFM, from 1995-2001. His intention in building this program was for residents to experience providing medicine in resource-poor areas and globally navigating the healthcare of the underserved.
Residents have the opportunity to travel to Kingston, Jamaica and Chulucanas, Peru, each year. These 1-2 week medical trips are for resident’s to experience new practice environments culture; they are available to all family medicine residents.
-

Street Medicine
Mount Carmel has a robust, distinguished Street Medicine program that has been operating for over 30 years. The Street Medicine track for Residents is comprehensive and includes longitudinal experiences starting in the first month of residency. Residents will regularly work on the mobile medical coach and with the outreach teams to meet individuals where they are and to provide high-quality care in various environments. As residents progress through their training, they will progressively spend more time with the Street Medicine team.
-

Women's Health
PGY-1 residents receive Advance Life Support in Obstetrics (ALSO) training and complete a rotation focused on prenatal care.
PGY-2 residents spend time in labor and delivery, as well an outpatient OB/GYN office under the supervision of a board-certified obstetrician, while receiving training in obstetrical management and gynecologic procedures.
Residents provide routine outpatient prenatal services to their pregnant patients in FM clinic, and have the opportunity to then deliver babies with a team of obstetricians who provide 24 hour attending coverage.
-

Geriatrics
PGY-2 residents complete a focused geriatrics rotation at the Chalmers P. Wylie VA Ambulatory Care Center under the supervision of geriatrics fellowship-trained family physicians.
PGY-2 and PGY-3 residents also receive longitudinal education in geriatric medicine by caring for patients residing in local nursing facilities under the supervision of St. Ann’s Family Medicine faculty. During these afternoon sessions, residents receive education via direct patient care, as well as geriatric-focused didactic sessions.
-

Pediatric Medicine
Our residents begin their pediatric education right from the start through the Pediatric Advanced Life Support (PALS) and Neonatal Resuscitation (NRP) certification courses during Immersion.
All residents complete four months of focused pediatric rotations through Nationwide Children's Hospital and one month in the newborn nursery at Mount Carmel St. Ann's.
In addition to these focused rotations, we also provide longitudinal pediatric experiences both in our FMC throughout all three years and at an outpatient Nationwide Children‘s primary care clinic one half-day per week during available rotations in the PGY-3 year.
-

Research & Scholarship
Quality improvement is a component of a physician's lifelong education. As such, our curriculum integrates quality improvement throughout the three years of residency in multiple ways.
Residents prepare and present journal club during didactics. They also complete an Ambulatory Pharmacotherapy rotation, working with our Director of Pharmacy Education to review pathophysiology and pharmacology of core conditions, perform prospective chart review, and implement their learning through informed discussions of risk/benefit with their patients.
A longitudinal quality improvement project is completed throughout the three years of residency. During second year, residents complete a dedicated Quality Improvement rotation, during which time is dedicated to starting or furthering a personal QI/research project. These QI projects are presented during at least one regional or national conference.
PGY-3 residents complete a Practice Management rotation that ties these experiences together. During this time, residents develop an evidence-based smart phrase or template to improve office efficiency.
Separate from the quality improvement research, each resident does in-depth research on a current topic in medicine. Topics are chosen by residents based on areas of interest and passion and are supported by faculty to complete a Grand Rounds presentation during PGY3 year.
Additional scholarship opportunities (including applying for grant funding, book chapter review, residency curriculum resource submission) continue to be offered and widely disseminated to residents and faculty for those interested in additional scholarship opportunities.
-

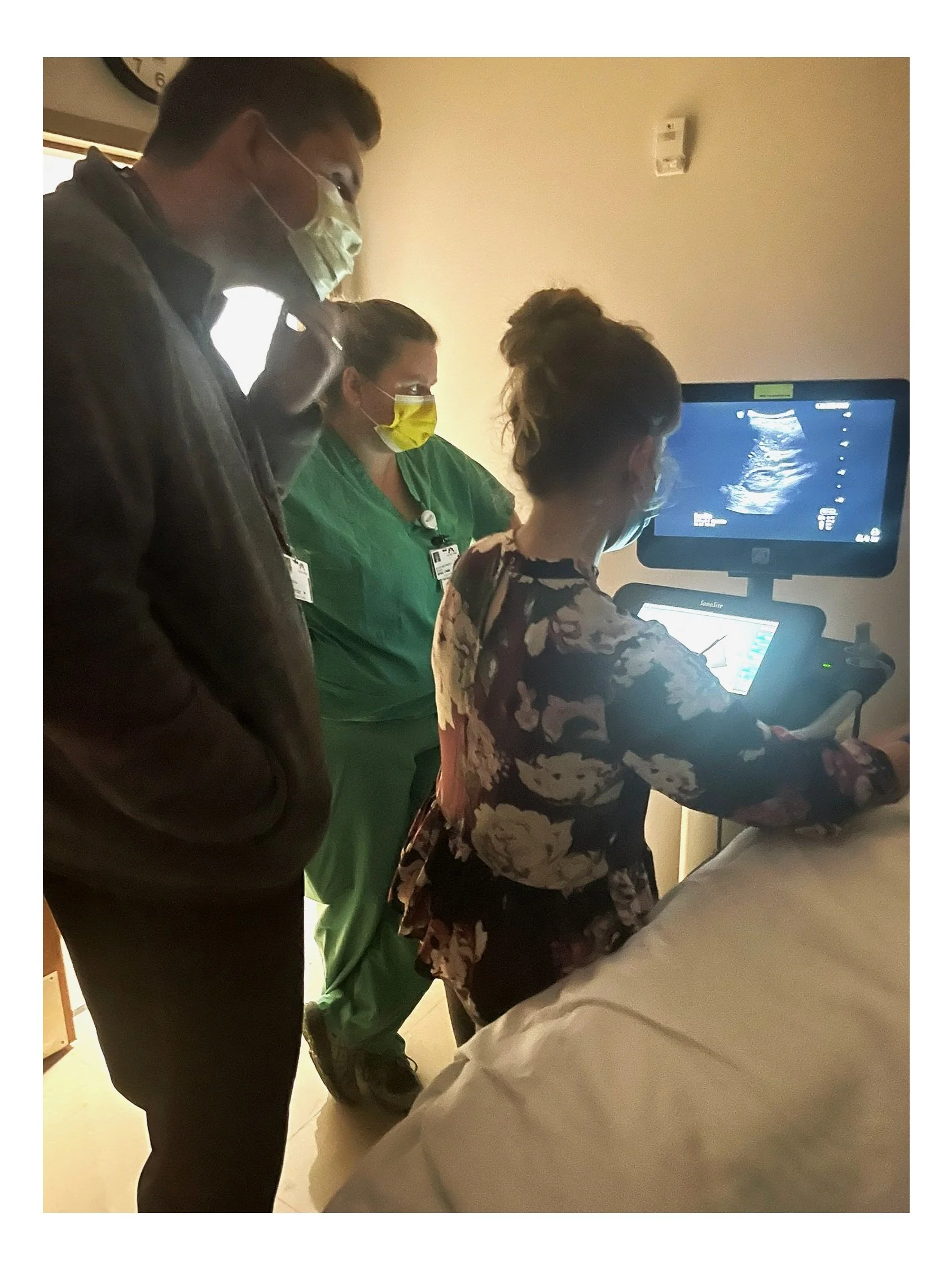
OMM
Residents gain increased knowledge and understanding of osteopathic principles and practices here at St. Ann’s Family Medicine. Our osteopathic residents incorporate OMM in their patient encounters with supervision provided by attending faculty.
An osteopathic lecture takes place monthly during didactics with the content of these lectures focused on taking the basic OMM skills and knowledge that you possess and focusing on a clinical diagnosis and how OMM can specifically be utilized to affect that disease process.
-

Behavioral Medicine
PGY-2s participate in a one-month rotation across the continuum of care in behavioral health, focused on identifying, understanding and responding to the mental health needs of patients from diverse backgrounds.
Residents experience a longitudinal curriculum throughout residency, which includes a series of lectures, case discussions, physician support groups and activities pertaining to human behavior, psychiatry, community medicine and electives in teen health and chemical dependency.
Key concepts of human behavior, psychiatry, and community medicine are learned throughout the year with involvement of the inpatient and outpatient services. Supplemental readings are provided. Residents also participate among various community programs to gain experience with the public health system, to understand community health issues and to become familiar with treatment interventions different community medicine programs offer to this population.
This structured interaction with the public health system provides residents opportunities for assessment of risk for abuse, neglect, and family and community violence.
Simulation Curriculum
Four times per year, residents have the opportunity to participate in simulated outpatient and inpatient scenarios, at the Simulation Center. The center is a dynamic, system-wide training center with a diversity of high-fidelity human patient simulators and clinical education resources. Residents have the opportunity to implement patient-focused team treatment, enhance quality of care and improve patient outcomes. Residents participate in suturing workshops, EKG interpretation, ultrasound, stroke simulation, to name just a few.
Elective Rotations
Each resident has six months of elective time between the PGY-2 and PGY-3 years. This time can be used in a variety of ways to support the specific needs and interests of each individual resident.
Our advisor program serves as a strong asset in this process. As a resident, you are expected to meet with your advisor once a month to discuss your progress, including your career goals and elective plans.
We utilize a detailed "Roadmap to Graduation", which assists both you and your advisor in strategizing your best path without missing any important requirements
Culinary Medicine
Residents participate in four Culinary Medicine sessions per year that follow the Tulane "Health Meets Food" Curriculum. Each session consists of a case-based lecture and discussion taught by Aimee Shea, Associate Professor of Nutrition at the Mount Carmel College of Nursing.
These case discussions are followed by a group cooking class where residents and faculty learn how to make nutritious recipes together, with the goal of taking these cooking tips to their own patient care encounters.
Topics have included: bariatric nutrition, pediatric nutrition, nutrition in pregnancy and breastfeeding, DASH diet and Mediterranean diet as treatments for hypertension, as well as discussion of weight bias.
Cooking classes are led by a Chef from "Local Matters", a community organization we partner with to increase education about food access, education and advocacy.